Vol 2 | Issue 2 | May – Aug 2016 | page:31-39 | Otman Benabdallah, Ahmed Khamlichi
Author: Otman Benabdallah [1], Ahmed Khamlichi [1]
[1] Centres hospitaliers de Tanger, Morocco
Address of Correspondence
Dr. Otman Benabdallah
Centres hospitaliers de Tanger, Morocco
Email: otman.benabdallah@hotmail.com
Abstract
Background: Utilized since 1951, the Boytchev procedure is an open anterior repair, performed for the treatment of anterior gleno-humeral instability, which involves rerouting the muscles that attach the coracoid process deep to the subscapularis muscle between this and the capsule. The tip of the coracoid with its muscles is reattached to its base in the anatomical position.
Method: We conducted a prospective study of twenty patients with recurrent shoulder dislocations who were treated by the Boytchev procedure. All are men, with an average age of 29.2 years (age range from 17 to 42 years). 14 patients were affected on the right shoulder, 6 on the left. All had a clinical history of recurrent dislocation . We also performed a search of all published articles in the literature (16),17 studies including our series, with the aim of estimating, via a statistical analysis, to shed light on the post-operative results of recurrent anterior dislocations of the shoulder, for determining the reliability of this technique and possible specific risk factors that might lead to recurrence.
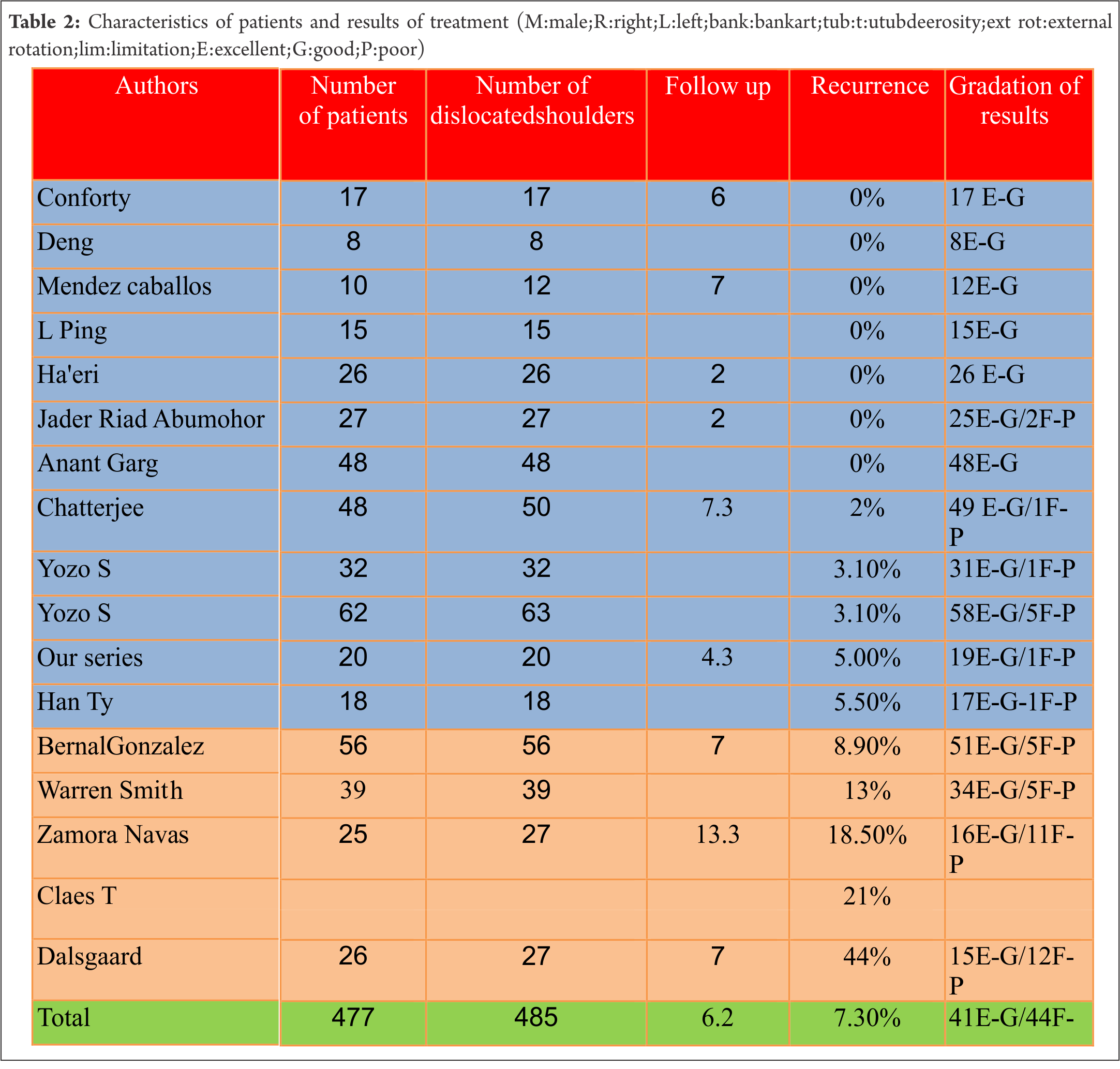
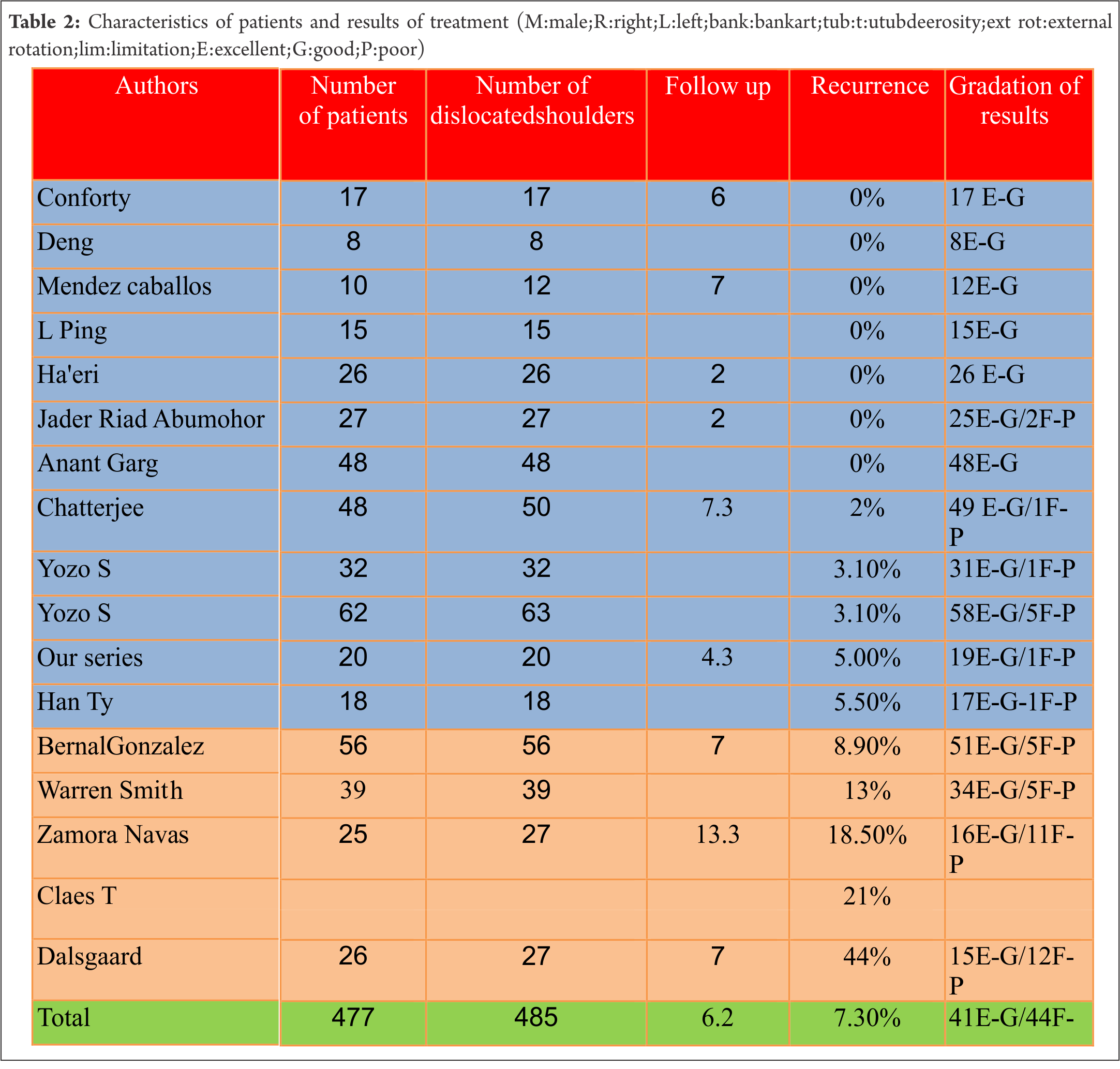
Results: Evaluated using the Rowe score in our series, 19 patients had excellent and good results; one patient, who suffered a recurrence, had a poor result in terms of stability. Another patient developed osteoarthrosis. For the 17 studies, the number of patients is 477 with 485 dislocated shoulders. The rate of recurrence is 7.33% .In 12 studies, the rate is 2%, versus 21.08% in 5 studies with a significant difference (1-p=99.89%). Concerning the gradation of results, we have 441 excellent and good results and 44 fair and poor (91% versus 9% with p=>99.9% which is also very significant).
Conclusion: The Boytchev procedure exhibits low recurrence rates in compiled studies and so can be considered a reliable surgical technique.
Keywords: Shoulder recurrent dislocation, Boytchev treatment
Introduction
Shoulder instability is one of most controversial joint diseases in terms of diagnosis and treatment. Clinical, anatomo-pathological, radiological, surgical and cadaveric findings have improved the recognition of unstable shoulder lesions and allowed a better understanding of their etiology and possibly a more adequate treatment. One of the key points about anterior dislocations is that Bankart is not always the essential lesion; lab tests seem to show in fact that this lesion alone does not frequently lead to dislocation, and it coexists with many other possibilities: HAGL lesions, capsular rupture or capsular plastic deformation, glenoid fracture or bony erosion, large Hill Sachs lesions, and muscular insufficiency. Now it is accepted that shoulder stability depends equally on static and dynamic stability, even after Bankart or capsular shifts [1]. The standard treatment is surgical; more than 150 surgical techniques have been used, and all are compromised by their own rate of recurrences and complications (loss of range of motion, osteoarthrosis, infection, etc) [2].
In our practice, we generally use the Latarjet or Bankart procedures. In 2002, we introduced the Boytchev procedure as another optional open repair for recurrent anterior dislocations [3].
This technique has also given rise to recurrences and complications; we note in the literature that a majority of authors obtained excellent and good results (Conforty, Ha’eri, Chatterjee, Shibata Yozo…), while others results were merely fair (Dalsgaard, Zamora-Navas) [2, 4, 5, 6, 7, 8]. Recurrence rates vary between 0% and 44%, so the procedure seems to be controversial.
Between January 2002 and December 2012, we therefore conducted a prospective study of 20 patients treated by the Boytchev procedure, with a follow up extending until December 2014. Our purpose was to shed light on the postoperative results of recurrent anterior shoulder dislocations after the use of the Boytchev procedure, to review the published articles in the literature and to compare these overall results with those obtained with other open repairs to determine the effectiveness or otherwise of the Boytchev procedure and to see if any specific risk factors can be identified which might explain the discrepancies already noted and settle the disagreements between those who have observed conflicting tendencies [7, 8]. It should nevertheless be recognized that comparing different open repairs is difficult because of a remarkable variability in study designs.
Material and methods
No funds were received in support of this study. All the patients gave their informed consent prior to being included in the study; the study was authorized by the local ethical committee and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki as revised in 2000.
For our present study, the patients were selected to meet the following criteria: clinical history of anterior shoulder instability as a result of a traumatic event, more than three episodes of shoulder dislocations, no clinical evidence of multidirectional instability, and eventual previous surgery to the injured shoulder for recurrent anterior dislocations, other than the Latarjet procedure.
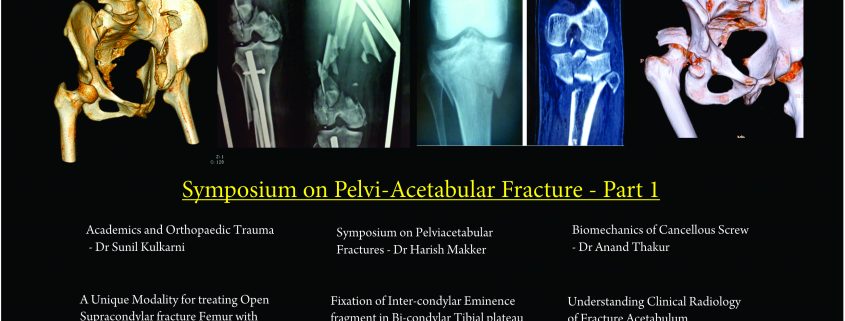
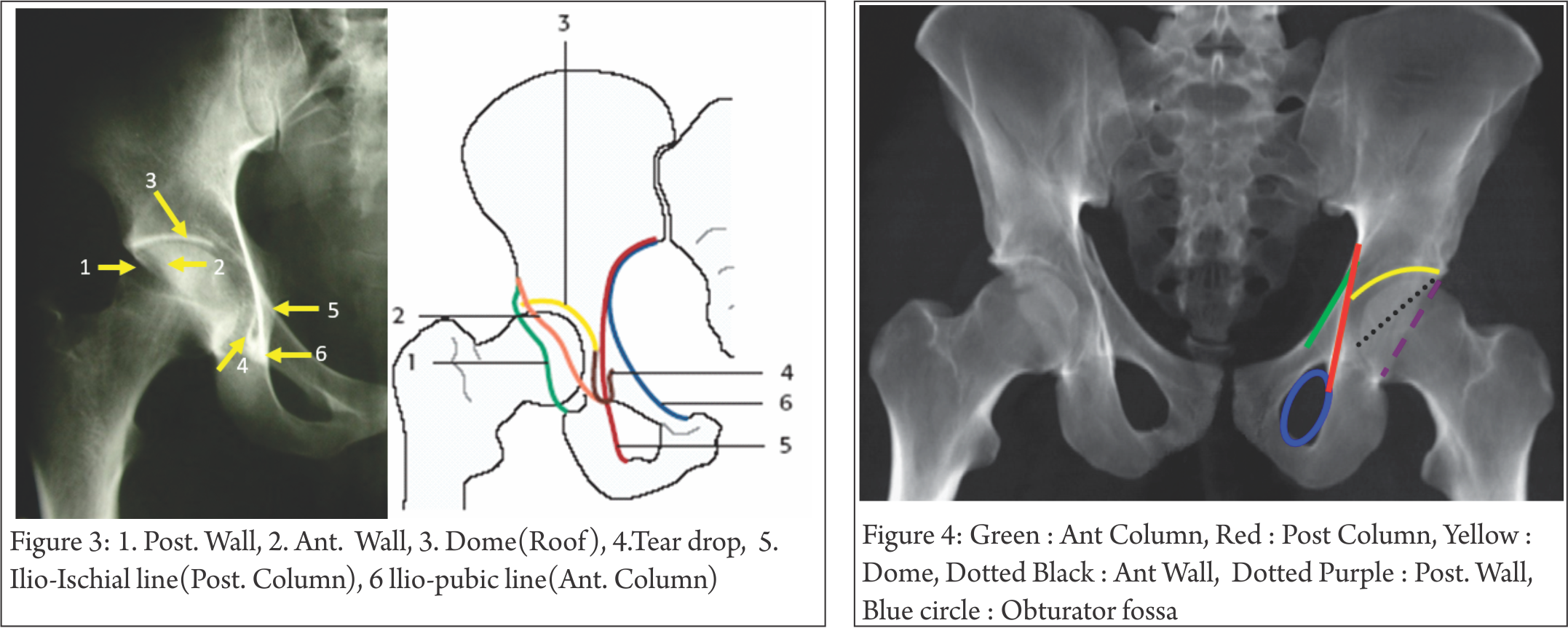
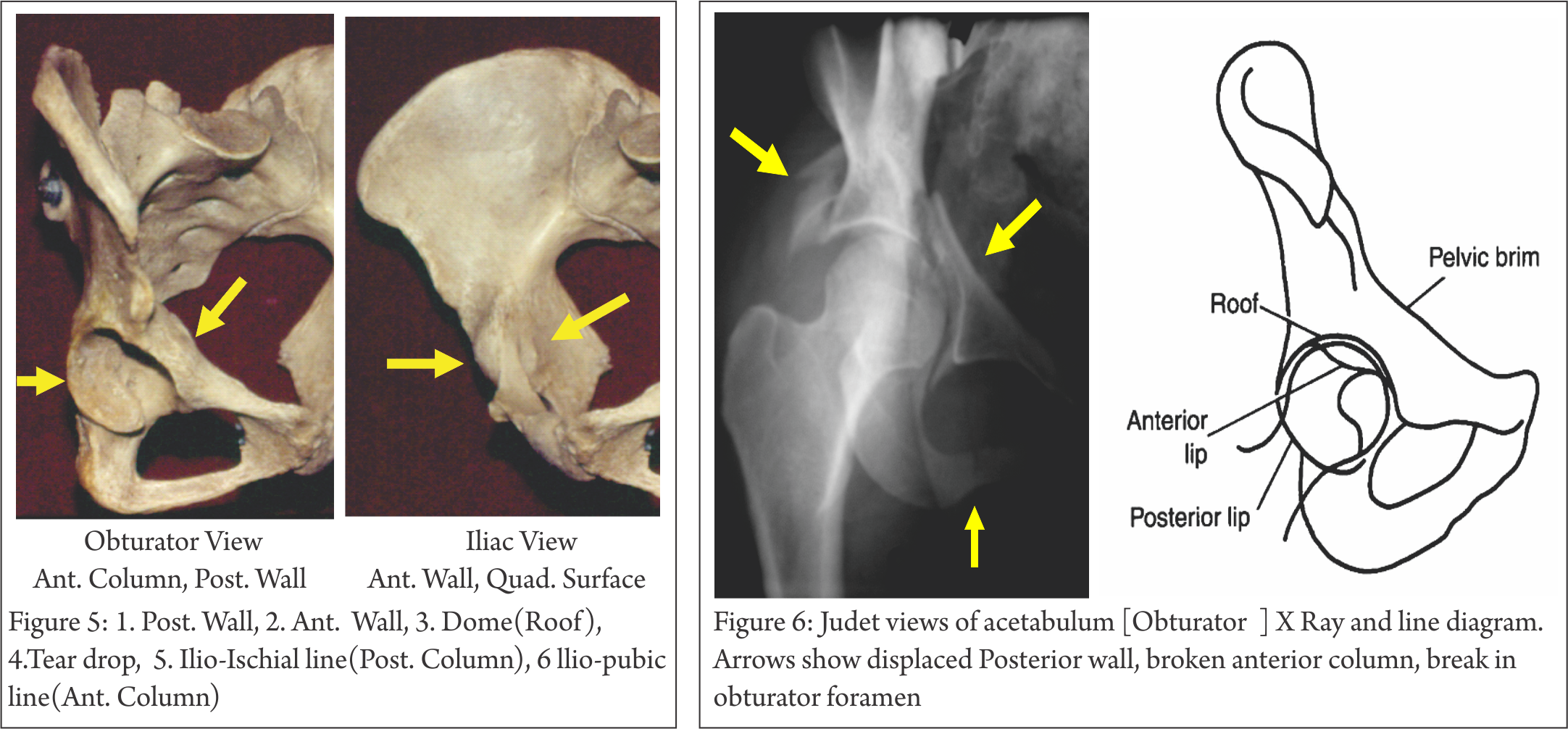
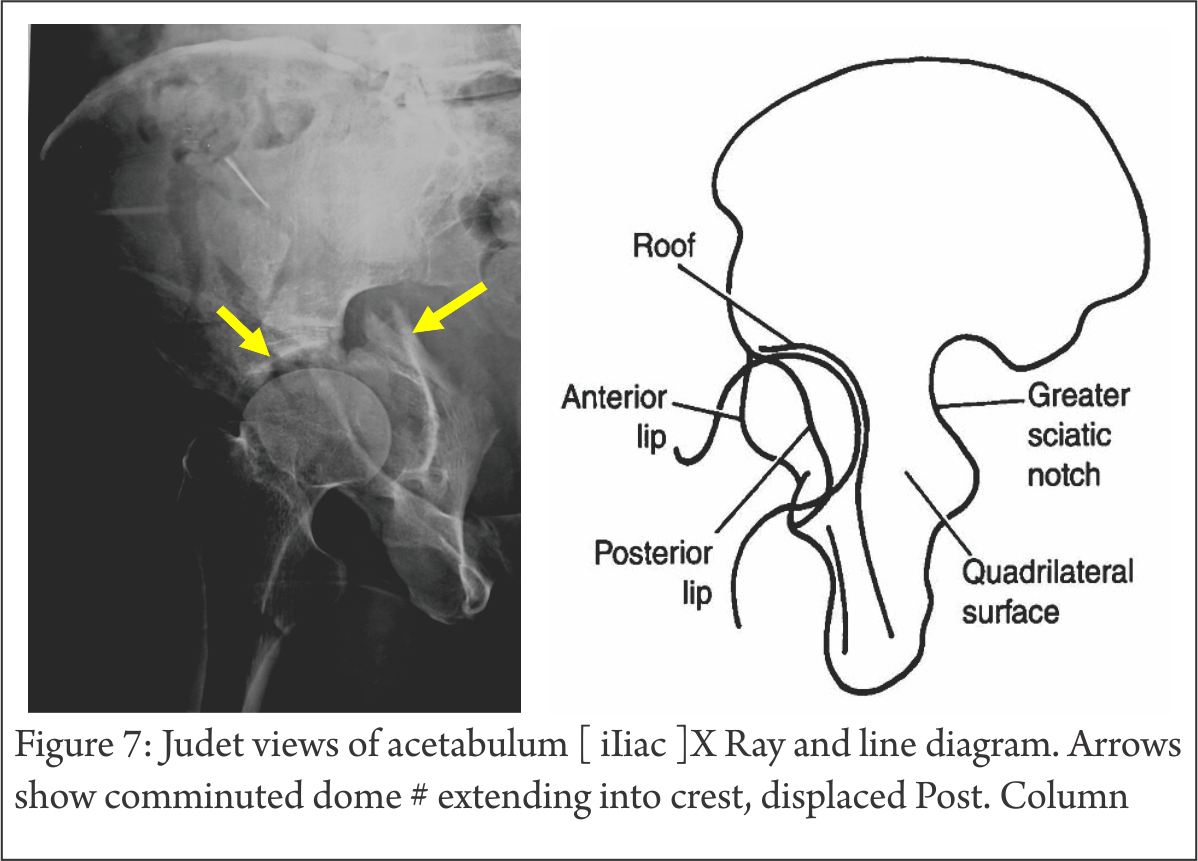
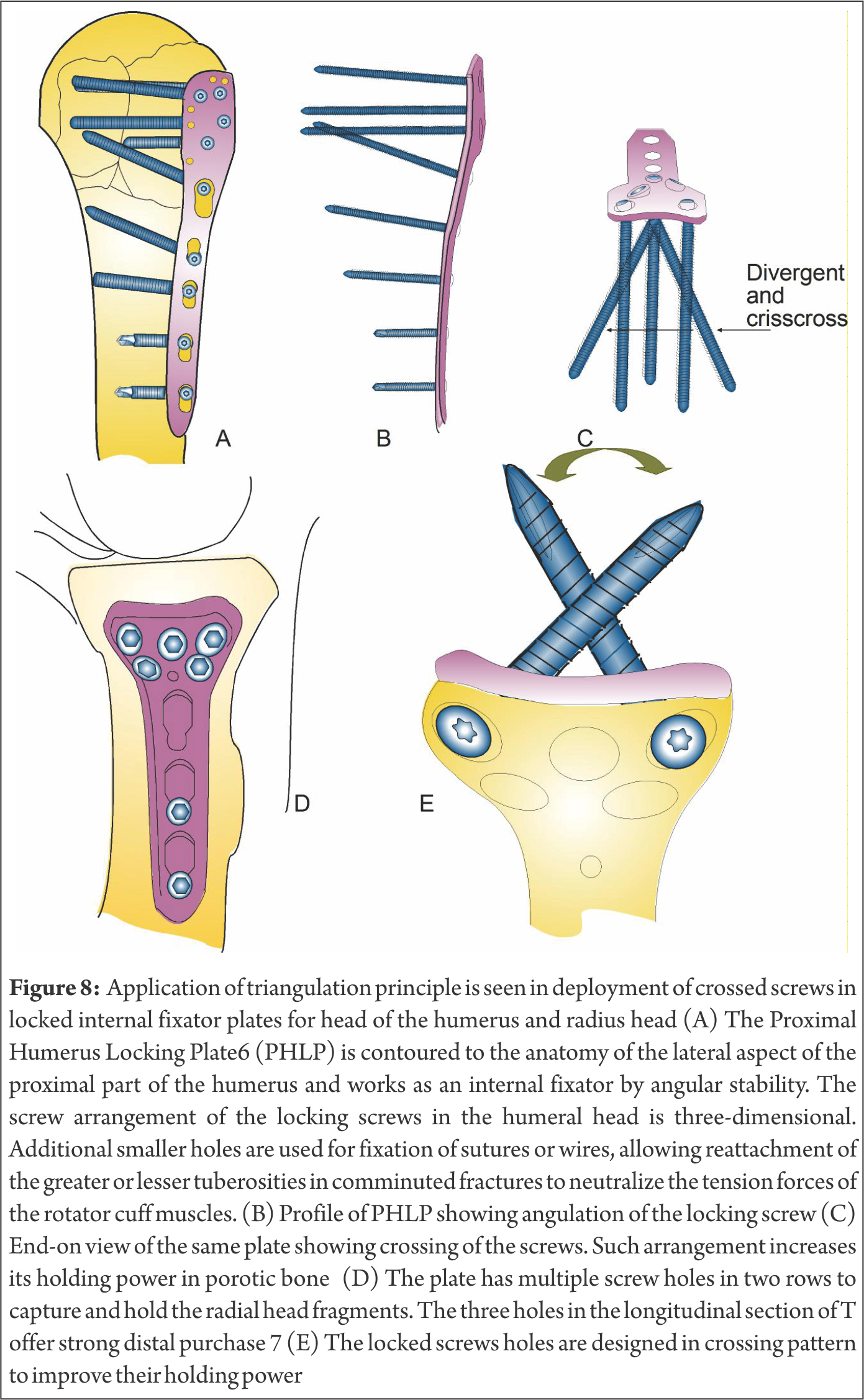
Twenty consecutive recurrent anterior dislocations of the shoulder were treated by the Boytchev procedure between January 2002 and December 2009. All twenty dislocated shoulders were in male patients; one female patient refused treatment. The average age was 29.2 years at the time of the surgical intervention, with an age range of 17 to 42 years. Fourteen patients were affected on the right shoulder, and six on the left; the right was the dominant side in all the patients. The total number of dislocations suffered by individual patients ranged between 4 and 200, with an average of 19 in a period of three to eight years. The etiology of the dislocation was related to a fall in thirteen patients and to sporting activities in seven patients. All had a severe initial traumatism; their first dislocated shoulder had been put back by an experienced practitioner and immobilized for periods ranging from a few days (the immobilisation being removed by the patient) to a few weeks (five days to six weeks).Three patients had a minor amyotrophy. No patient had generalised ligament laxity. There were no spontaneous dislocations in our patients. All patients had some pain, but nine of them had significant episodes of pain, probably after subluxations, and all had positive apprehension tests and a feeling of instability and /or insecurity of the shoulder. Thirteen shoulders had a normal preoperative range of motion, while just one had restriction of elevation and external rotation; this patient had had previous surgical treatment using another procedure which had failed, the cause being an unhealed Bankart lesion diagnosed by arthro-scan. Four Hill-Sachs lesions and greater tuberosity fractures were diagnosed preoperatively by plain radiographs (frontal, profile, special radiographs, and sometimes CT scan or Magnetic Resonance Imaging (MRI). The follow up evaluation consisted of a clinical examination and radiographs (plain radiographs and/or special radiographs and/or computed tomography or Magnetic Resonance Imaging (MRI)). The Rowe score for instability of the shoulder, evaluating stability, motion and function and interpreting the results as excellent (100-90), good (89-75), fair (74-51) or poor (50 or less) was used for the results [9],(Table I).
Concerning the statistical analysis, we conducted a statistical analysis comparing the results of all published articles about the Boytchev procedure for treatment of recurrent shoulder dislocation. Using Pubmed, Cochrane, Lilacs, Japan Links Science, Index Copernicus, and Google Scholar, we performed a search of all published articles. 17 studies (14 published works, our own study and 2 cited by Dalsgaard) met the inclusion criteria with data about number of patients and number of recurrences of dislocation, which is the main concern here, follow up and gradation of results [7,10]. Our purpose is to estimate the true effect size using descriptive statistics to describe quantitatively the features of the data which may enable comparisons for the recurrence and results across the overall set of patients and dislocated shoulders and a multivariate correlation and regression tests between those variables, using XLStat, Sphinx Lexica and R softwares.

Operative technique
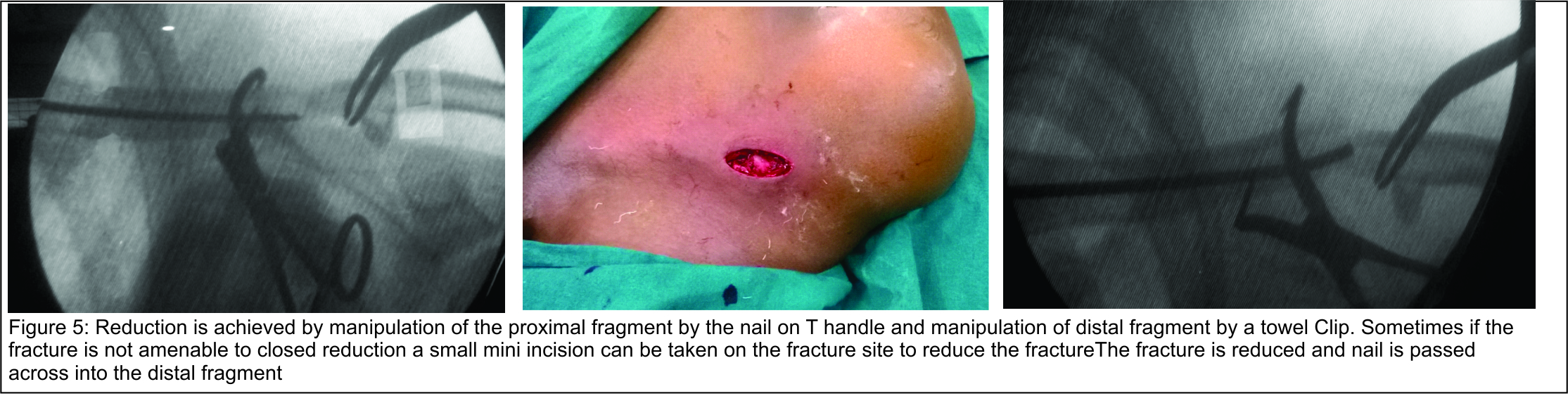
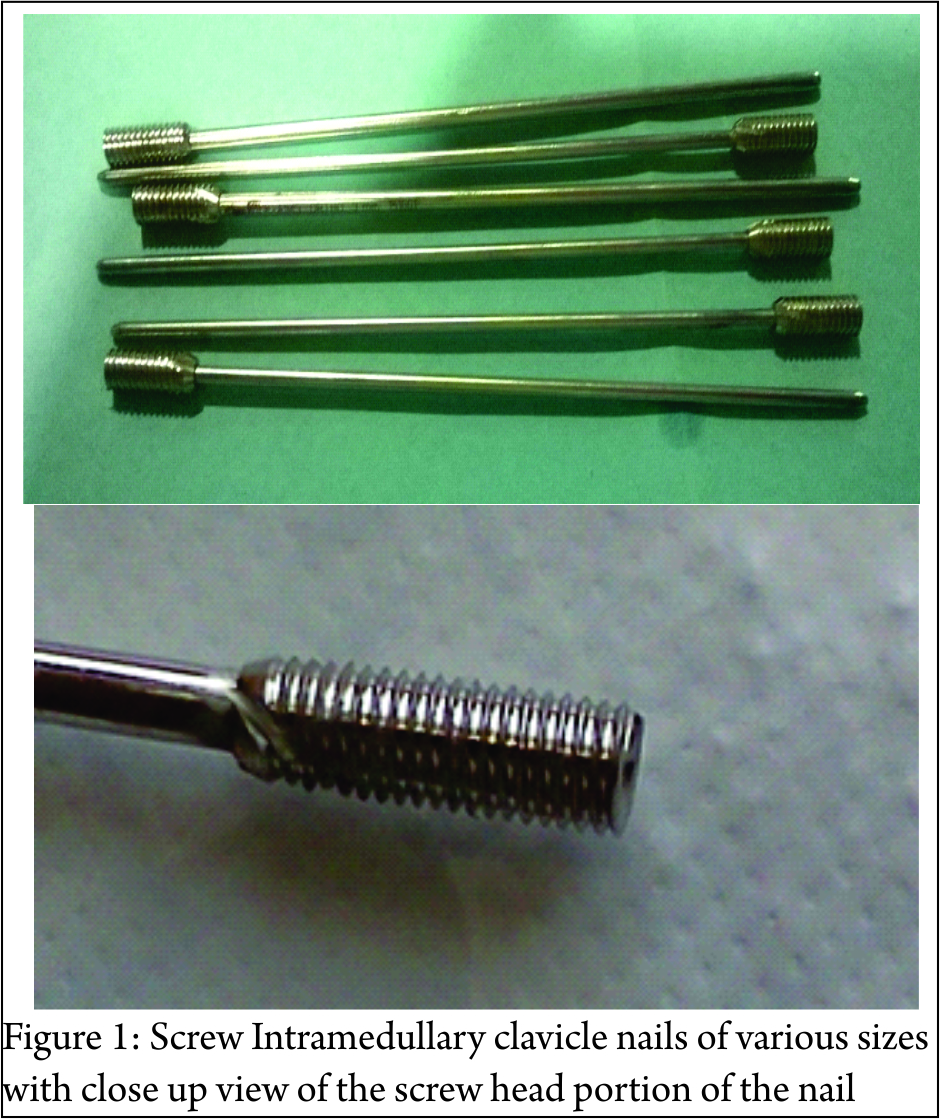
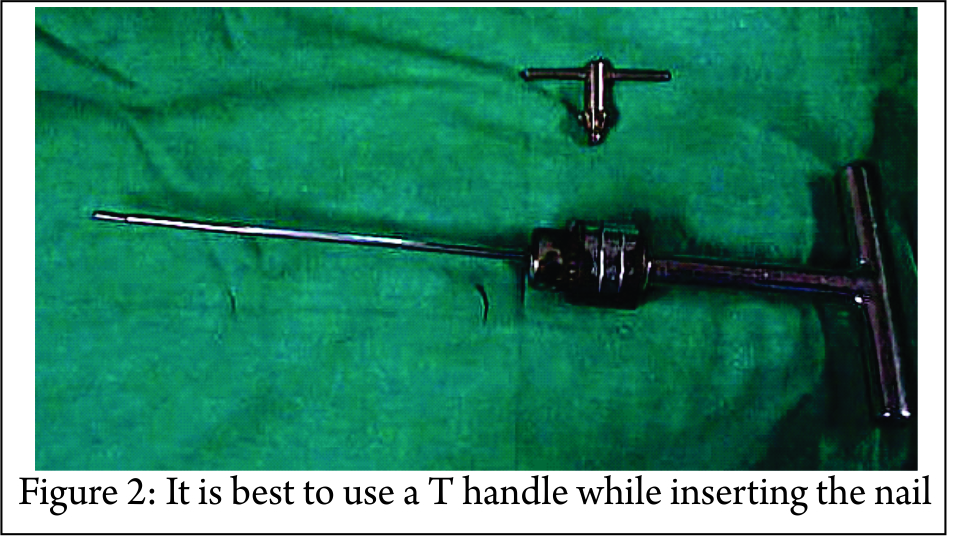
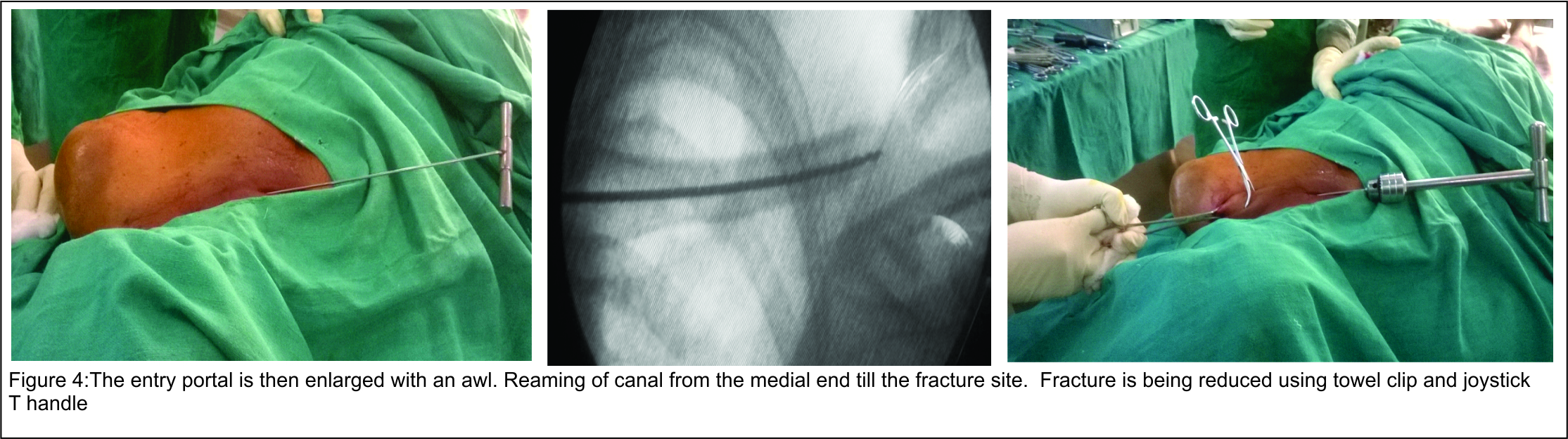
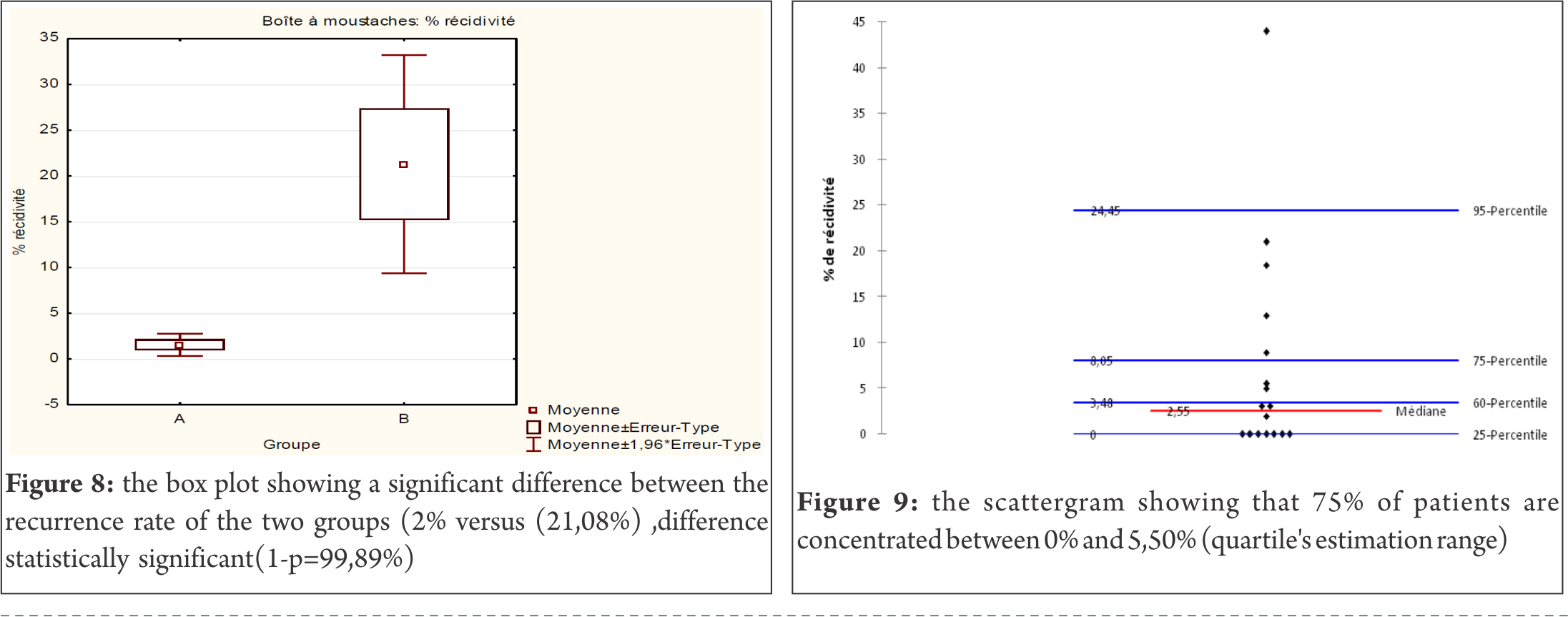
The incision begins from the level of the coracoid process, extending distally. We expose the horizontal part of the coracoid process with the tendinous origin of the short head of the biceps and the coracobrachialis muscle. An anteroposterior drill hole is made from the anterior end of the horizontal part of the coracoid process along its axis. The anterior 2 cm of the coracoid process is divided with an osteotome and mobilized distally gently to avoid a musculo-cutaneous injury (Fig.1) On the lower border of the subscapularis, we create a tunnel between shoulder capsule and muscle with a curved vascular forceps (Fig.2) (when the tunnel is created, we test the elasticity of the subscapularis introducing the fifth finger in the tunnel while making rotational movements), through which the isolated coracoid process with the conjoined tendons (Fig.3) is passed before being fixed to the predrilled proximal coracoid process with a 3.5 AO screw. The wound is closed in layers around a suction drain. A well padded dressing is applied. The arm is immobilized at the side of the chest with an elastic bandage.

Post operative management
During immobilization, isometric muscular reinforcement is begun. After removal of the elastic bandage, normally after three weeks, shoulder exercises are recommended. These are passive and active exercises, with special attention being paid to external rotational movement. (We did not recommend it immediately, but 4 weeks after open repair). All the movements are increased progressively by the patient himself and with the kinesitherapist for as long as is necessary to ensure recuperation of muscular strength, motion and proprioceptive control.
Results
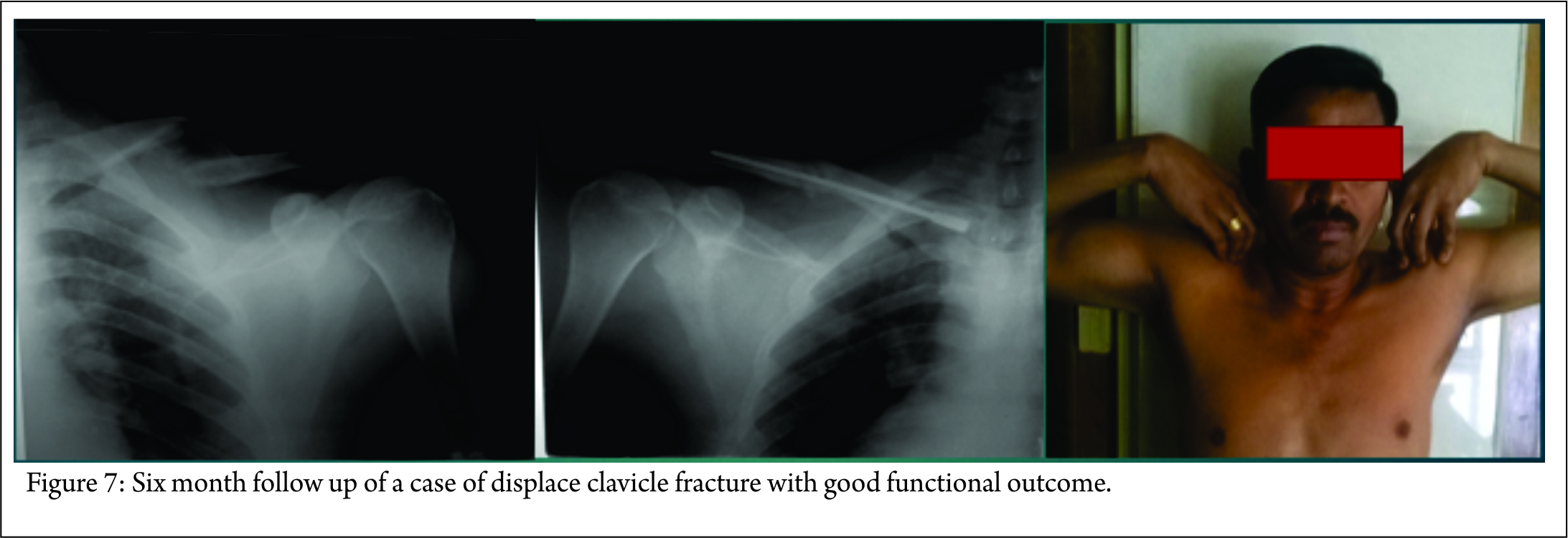
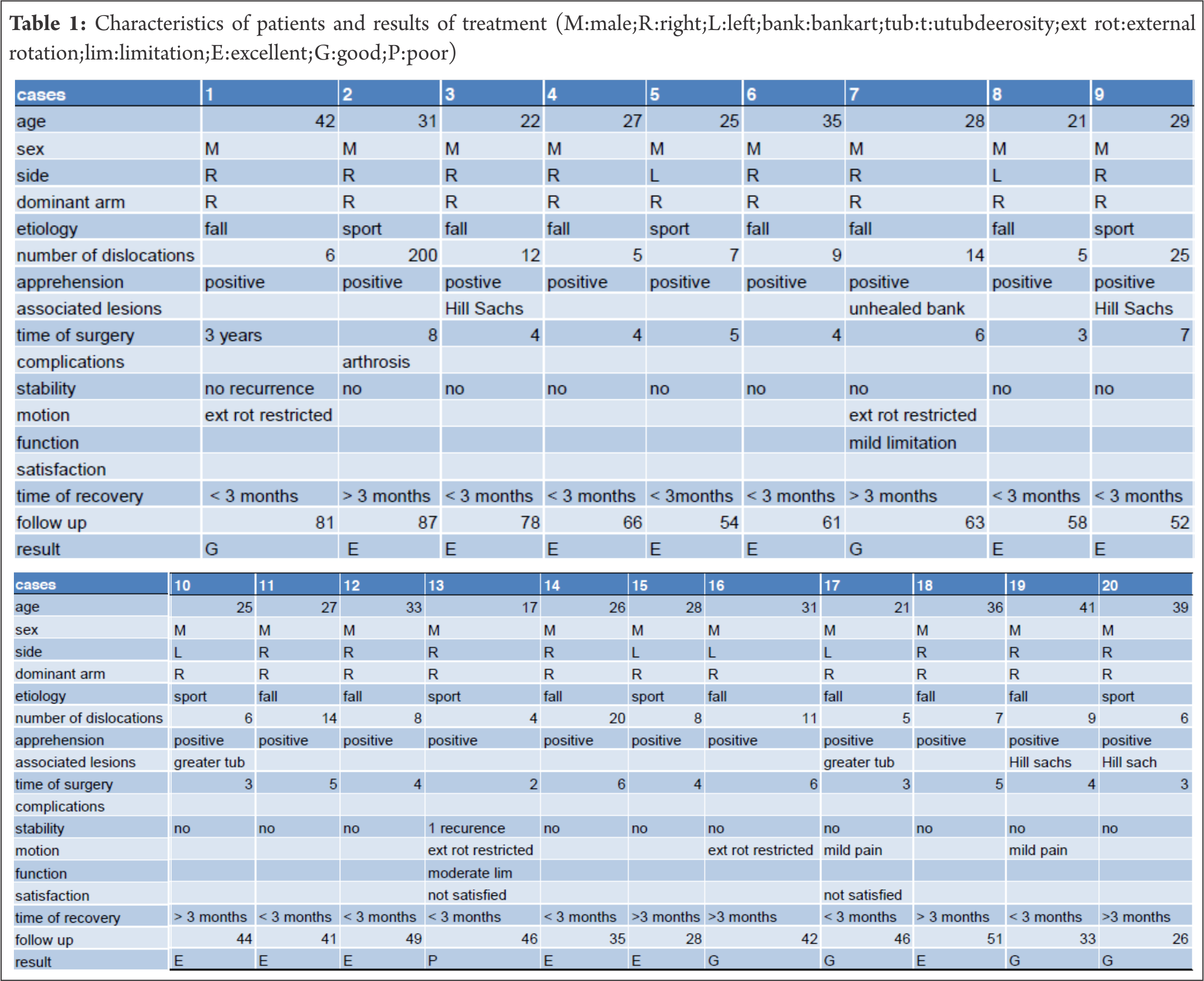
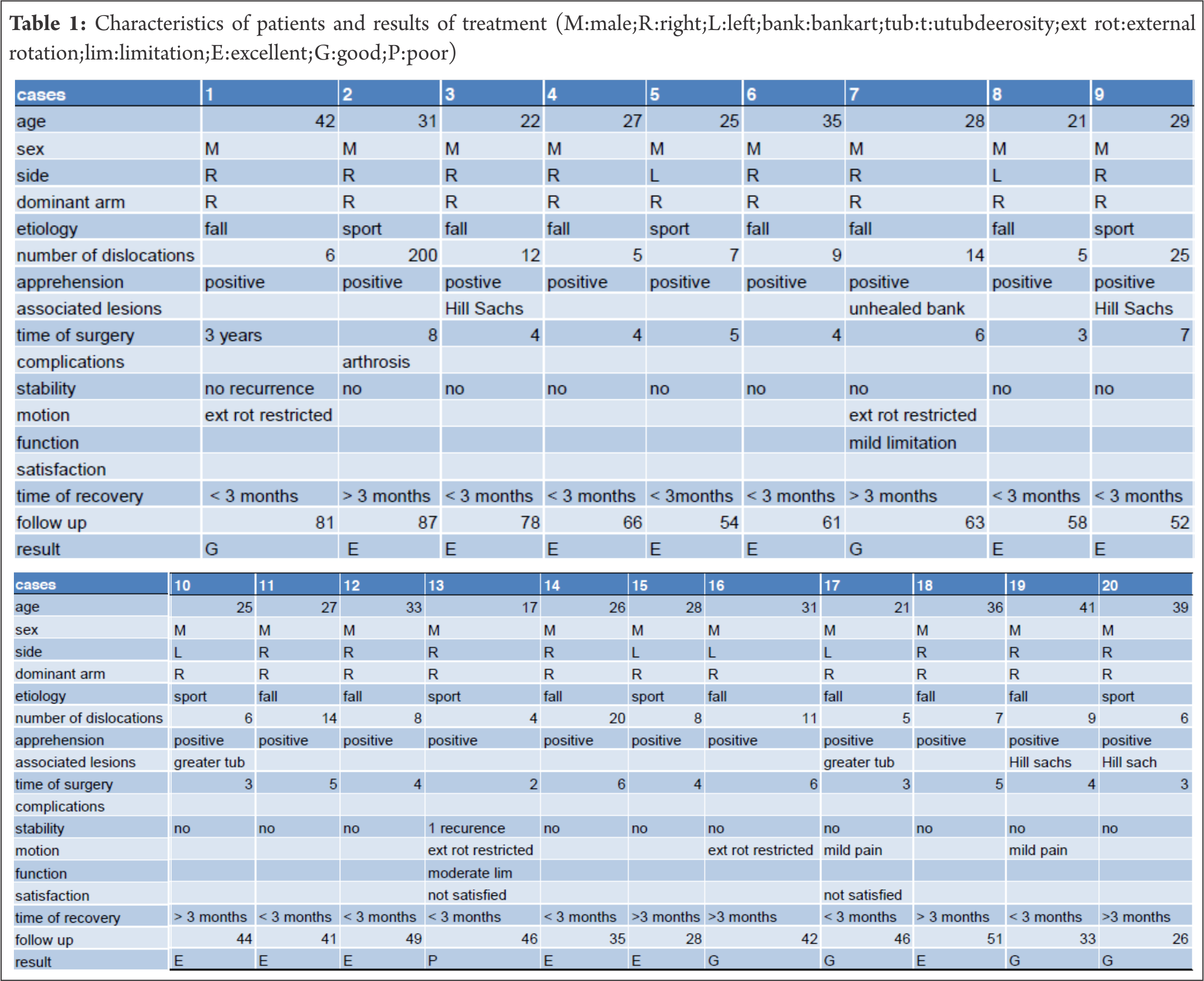
In our series, the follow up period varied from 25 to 87 months, with an average of 52.05 months (4.3 years). Nineteen shoulders showed excellent and good results (Fig. 4); one showed poor results. No complications such as infections or neuro-vascular injuries were observed. One patient developed a glenohumeral osteoarthrosis, and at the seven-year follow up, the latest radiographic examination showed the arthrosis (Fig. 5) to be evaluated as grade 2 on Samilson and Prieto’s scale; however, function was not affected [11]. Full mobility of the shoulder was retained in 16 cases, except for some minor restrictions of external rotation: 15 degrees in three patients and 25 degrees in one. The recovery period ranged from less than three months in thirteen patients to more than three months in seven patients. Recurrence occurred in one patient (Fig .6) after a high-level traumatic event eleven months after surgery. On physical examination, this patient actually had subjective apprehension but no sign of abnormal positive apprehension; this patient was not satisfied, but he is now stabilized three years after surgery. 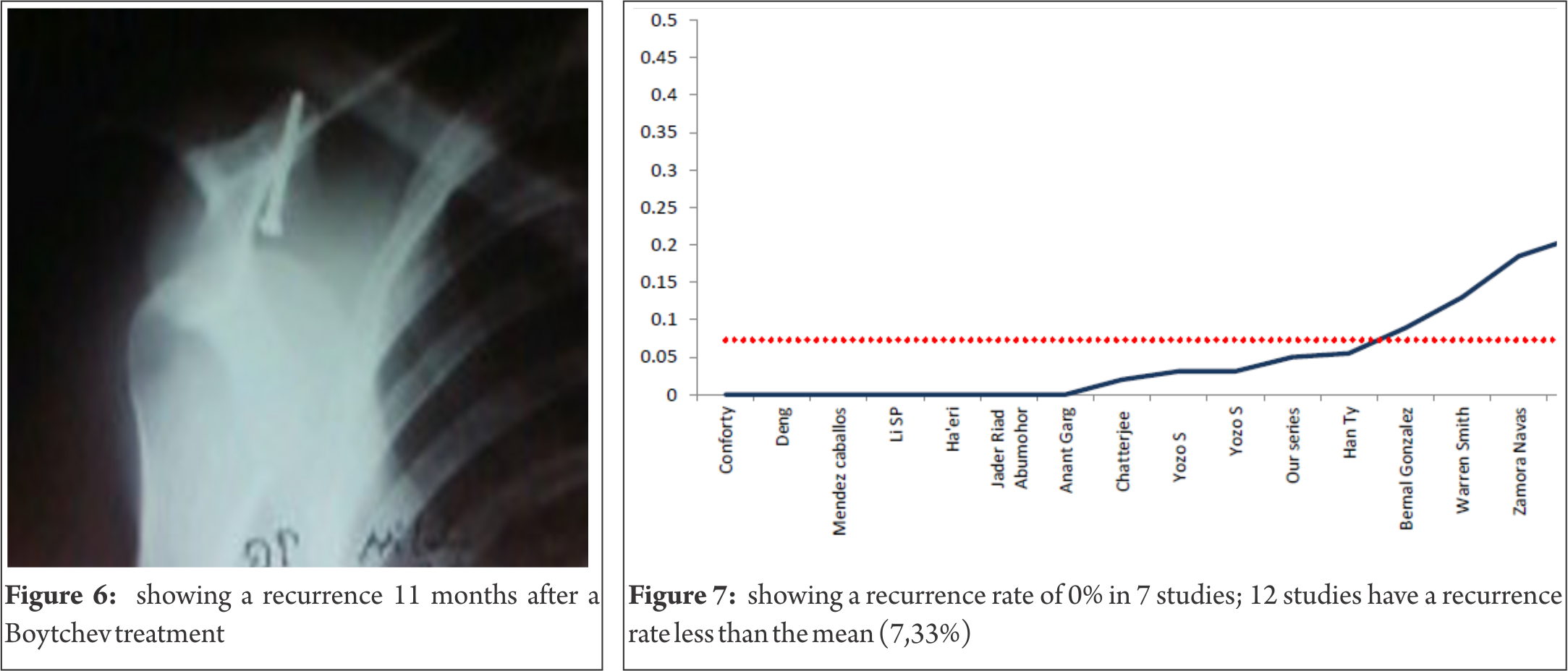
None of the patients complained of any significant pain (three patients complained about mild pain). All the patients were able to return to their normal activities (initial occupation or sport; seven were able to practise sport at more or less the same level).
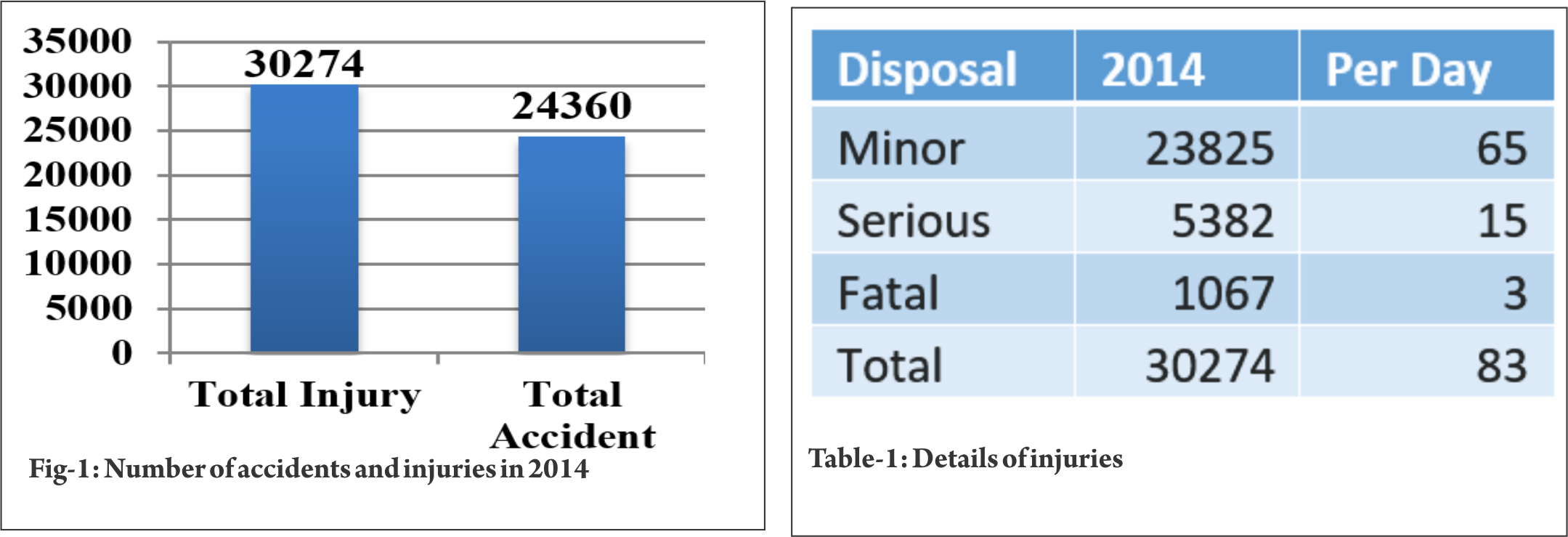
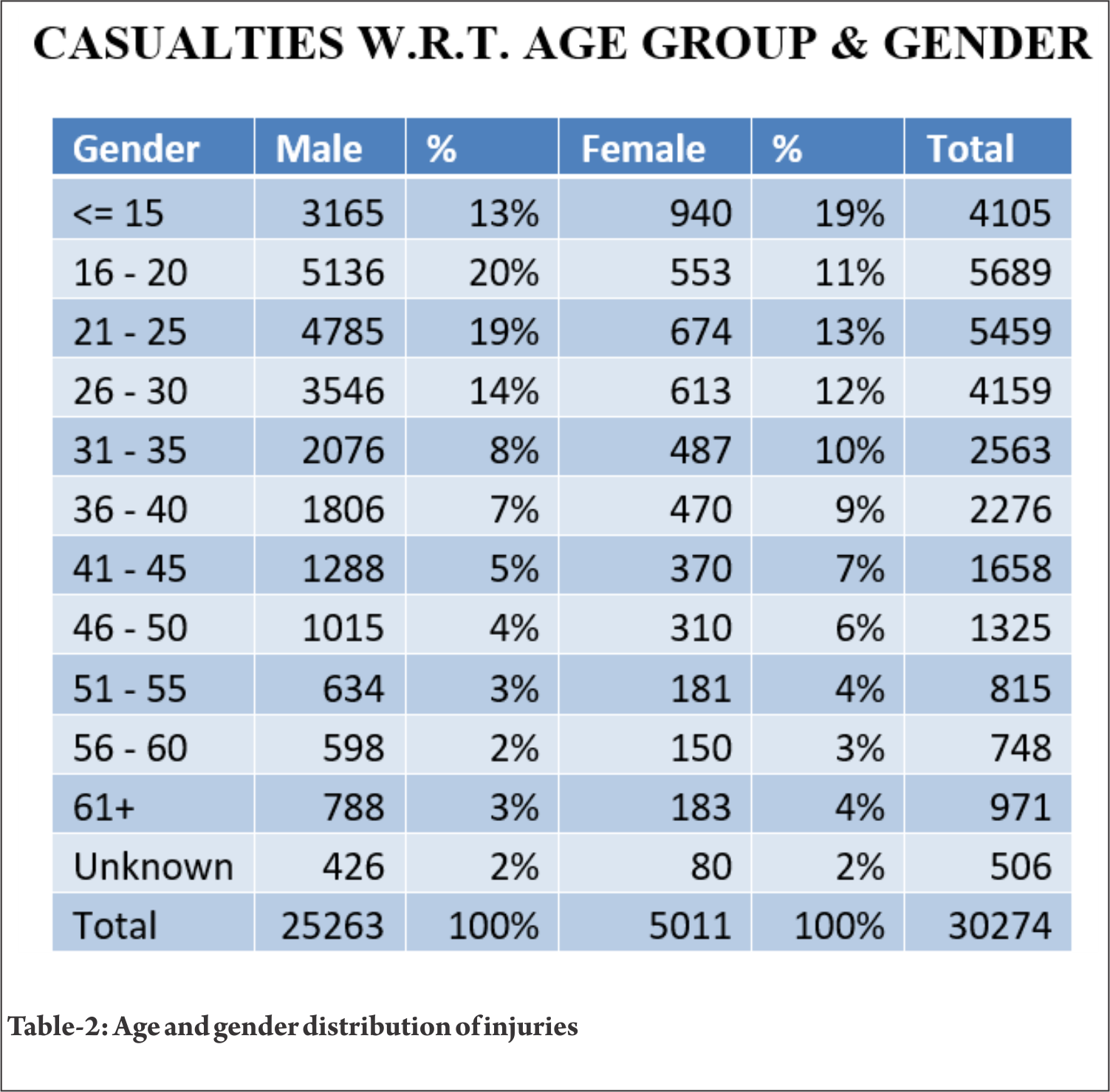
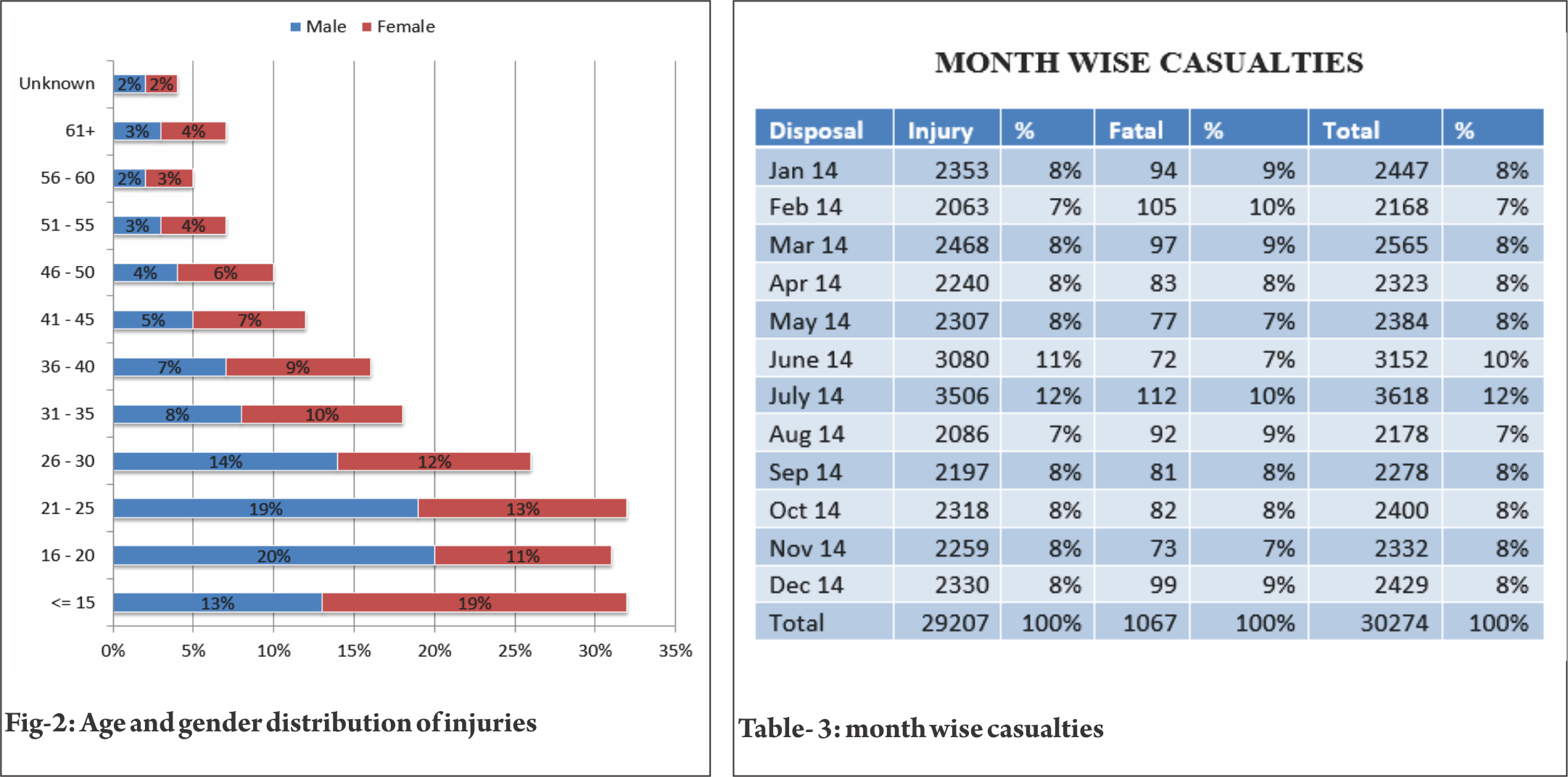
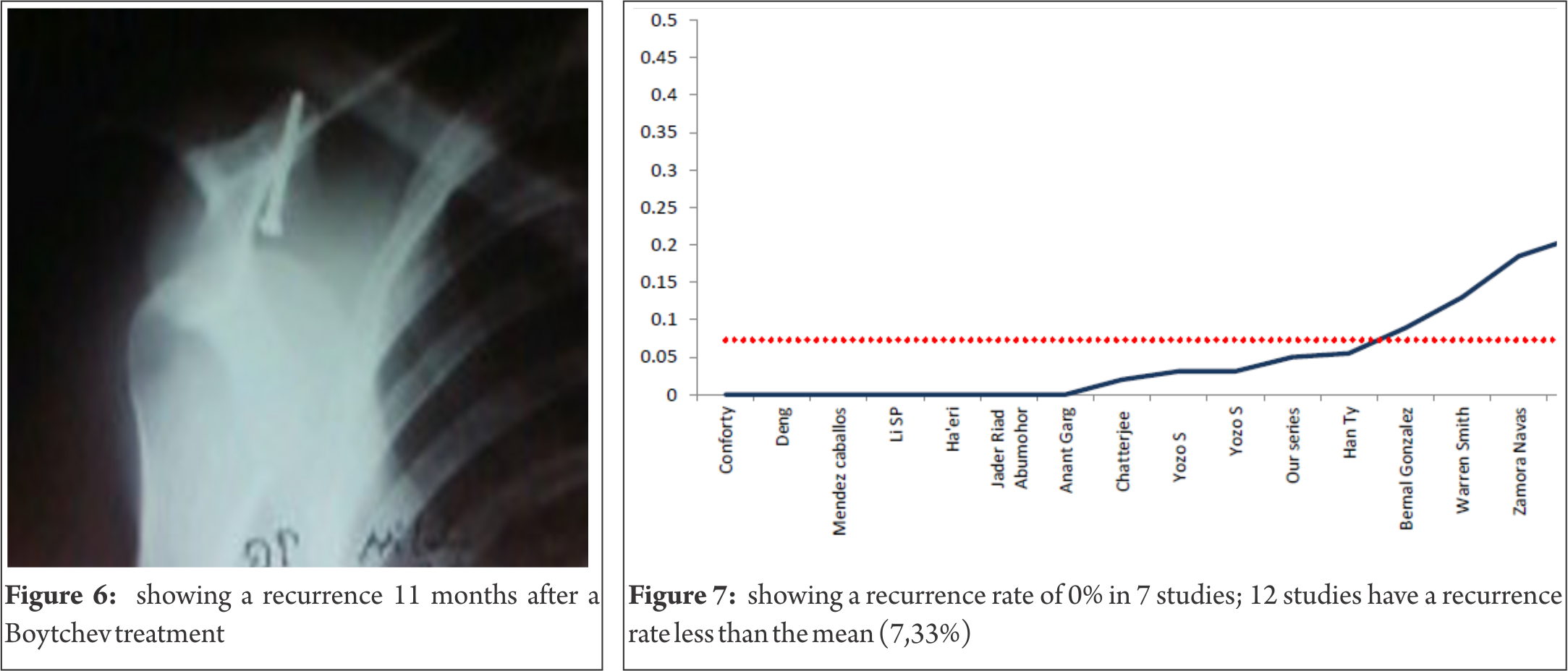
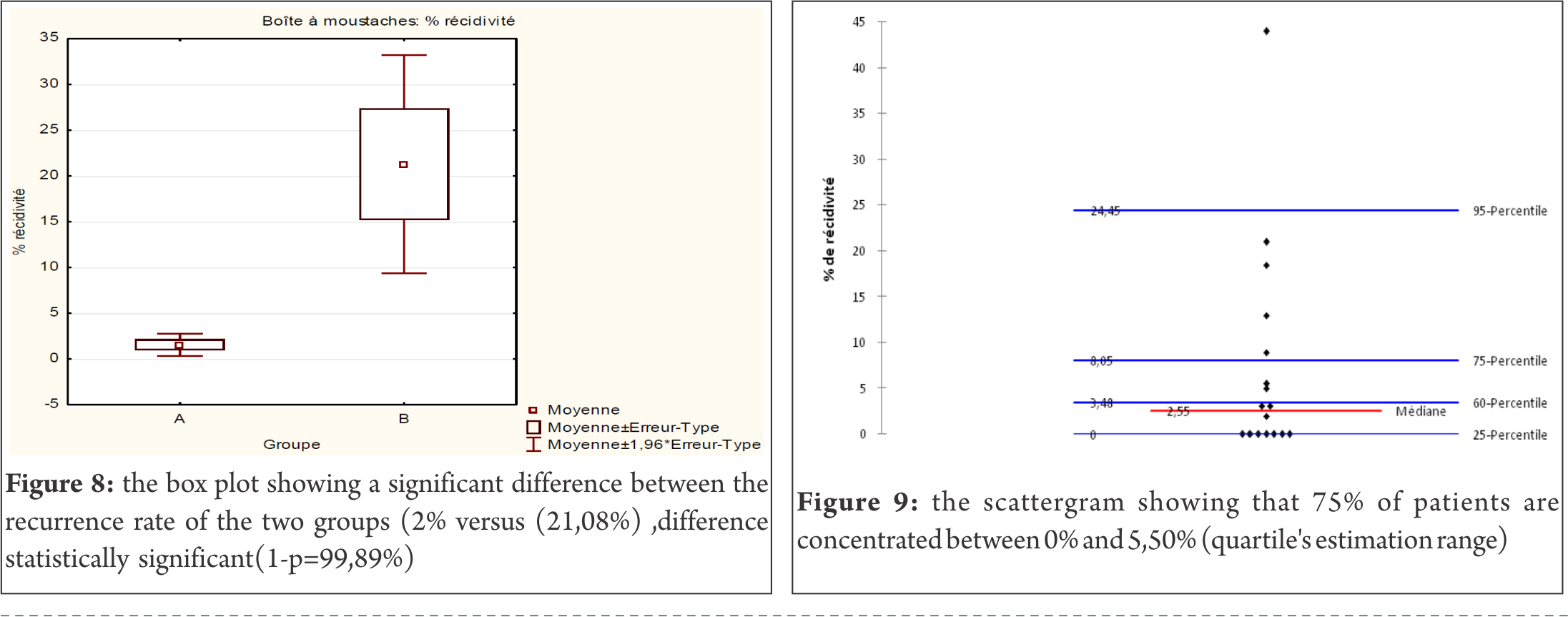
As for the statistical analysis, among 477 patients with 485 dislocated shoulders, the overall outcome of recurrence ranges from 0 to 44%; we show a minimum of 0% in 7 studies (41.18%), a maximum of 44% in one study (5.88%) (Fig.7), a range of 44, a median of 3.1%, a mean of 7.33% with a standard deviation of [1.354 – 13.246] for p= 0.05 or7.33+-5.946). In 12 studies or 75% of dislocated shoulders, the recurrence rate is less than 7.33%, the percentage is 2% versus 21.08% in 5 studies, a difference which is statistically very significant (1-p=99.89%) (Fig.8). The statistical measures of dispersion show a robust index (Q1=0, Q3=8, 90, distance=8.90) for the interquartile range, the skewness value is -2.106, the kurtosis value is 4.006. The frequency and density distributions have a high incidence and range between 0 and 6.44% in 12 studies (71%) and the quartile’s estimation range between 0% and 5.50% in 12 studies (75%) (Fig.9). Concerning the gradation of results, we have 441 excellent and good results and 44 fair and poor (91% versus 9% with p=>99.9%), a difference which is also statistically very significant (Fig.10). The Pearson’s coefficient correlation with a level of signification alpha = 0.05 between the number of dislocated shoulders and excellent and good results has a p-value =0.000 versus a p-value =0.666 for fair and poor results. The regression test between the number of dislocated shoulders and excellent and good results has a high coefficient of correlation (0.97). Finally, regarding the time interval of recurrence in 12 studies, it varies from 1 to 43 months, with a mean of 31 months. The follow up time varies between 1.7 and 13.3 years, with a mean of 5.25 years.
Discussion
The twenty shoulders with recurrent anterior dislocations treated by the Boytchev procedure in this present prospective study were followed clinically and radiologically for periods ranging from a minimum of 2 years to a maximum of 8 years. Analysis of demographic data shows that all our patients are men in the third decade of life, whose activity requires moderate or extensive use of the shoulder joint, and whose dominant right shoulder was that affected by the recurrent dislocation. Almost all the results are excellent, except for the one instance of recurrence. The stabilisation of the shoulder by the Boytchev procedure allowed most patients to return to their former level of activity. One patient developed a glenohumeral arthrosis wiithout effect on function. Like the majority of the authors who have reported on this technique, we thus confirm that the Boytchev procedure seems not to be affected by variables such as gender, age, dominance, number of dislocations, direction and severity of traumatism, rehabilitation, and function over time [2, 4, 5, 6, 12, 13, 14, 15, 16, 17, 18].

As for the statistical analysis, to our knowledge (based on the literature) this is the first quantitative comparative statistical analysis of studies for the treatment of recurrent dislocation of the shoulder by the Boytchev procedure. 17 studies which reported the main factor which is the recurrence were included in our systematic review, in which we also extracted data on number of patients and dislocated shoulders, follow up, time interval of recurrence, and gradation of results, and we pooled the outcomes whenever possible. First, we took the outcome of recurrence for efficacy assessment, and we found no significant dependence between the number of dislocated shoulders and the rate of recurrence, the coefficient of correlation being +0.06, but there is a robust coefficient of correlation (+0.97) between the number of dislocated shoulders and excellent and good results; the dependence is a significant linear correlation (Fig.11). On the contrary, the dependence is not significant between the number of dislocated shoulders and fair and poor results (Fig.12), the coefficient of correlation being +0.26 (barely influential). Concerning the gradation of results, we have 441 excellent and good results and 44 35 fair and poor results or 91% versus 9%, a difference which is obviously very significant with an interval of confidence of 95%, with t=6.17 and p=>99.9. The multivariate analysis of regression concerning the number of dislocated shoulders compared to the rate of recurrence, the percentage of excellent and good results and the percentage of fair and poor results confirms the robust correlation between the number of dislocated shoulders and the number of excellent and good results compared to fair and poor results (Fig.13). So we can confirm the existence of two different groups with the probability of 0.87% to reject the hypothesis that the groups being compared differ to a degree greater than would be expected by chance.

Elsewhere in the literature, Chatterjee, in a 7-year follow-up study, reported one immediate recurrence after surgery, while Zamora-Navas, in his long term study, reported an 18% recurrence rate, recurrences occurring between 4 and 43 months later (a short or medium period after surgery) [2 ,8]. Warren-Smith found 13% of patients complaining of episodes of possible subluxation at an average of 14.3 months after operative treatment [19]. Finally, Dalsgaard, with the same period of follow up as Chatterjee (7 years), observed a high rate of recurrence (44%) [2, 7]. Dalsgaard did not report the time interval of recurrences following surgical repair and insisted on the fact that the surgical treatments were performed by 11 different surgeons; is this an inhomogeneous parameter for the study? We cannot grasp the reason for this discrepancy; Dalsgaard comments that the technique needs more study [8]. Concretely, we note a mean recurrence rate of 7.33%. Like most authors , we consider this result very acceptable [2, 4, 5, 6, 12, 13, 14, 15, 16, 17, 18], (Table II).
Some published reports on the incidence of recurrent dislocations after anterior repairs by procedures other than the Boytchev procedure cite rates ranging from zero to 30% [20, 21, 22, 23]. In 1976, Morey and Janes, in their study of 176 patients, found a redislocation rate of 11% [21]. The operative reconstructions were of the Bankart and Putti-Platt types; in 7 of the 20 patients, redislocation occurred two years after surgery. In 1984, Rowe et al reported on the management of 32 patients with recurrence of instability; 84% had not had effective repair of the Bankart lesion at the initial surgery [9]. In 1988, O’Driscoll and Evans, who followed 269 consecutive staple capsulorraphies, found that 21% suffered redislocation [22]. In 1995, Ungersbock and then Zabinski reported similar findings (unhealed Bankart lesions) [24, 25]; Karlson, reporting on Bankart repairs, found a recurrence rate of 15% after arthroscopic repair and 10% after Bankart open repair [20]. It should be noted that many of these reports did not include recurrent subluxation or recurrent apprehension. The incidence of recurrence is also underestimated by some studies and revealed by Rockwood and Roca Ramos Vertiz [26, 27] We may also note that in the literature the recurrence rate did not always increase with follow up for different procedures [28, 29]. Hovelius did not observe a significant difference in recurrence rates at two, five and ten years follow up after surgery on recurrent dislocated shoulders [28]. Rowe reported that 52% of the dislocations recurred within two years after operative procedures [29]. This is not the case with the Boytchev procedure reported in the compiled studies in the literature [2, 4, 5, 6, 12, 13, 15, 16, 17,18].
The results of anterior repair by the Boytchev procedure or by other procedures cannot be evaluated solely in terms of the rate of recurrence, even though the avoidance of recurrence is the aim of stabilization. Rather, we must place the treatment of recurrent instability in its overall context. Surgical repairs of glenohumeral instability may lead to a number of complications which can compromise the final result. These include limited range of motion, deep infection, recurrent post-operative instability, failure of diagnosis (it is essential to differentiate TUBS syndrome and AMBRII syndrome), muscle laxity or weakness of the subscapularis, neurovascular injuries, hardware complications and secondary degenerative disease. Limited range of motion has been reported after Magnusson Stack, Putti Platt and other procedures. In 1979, Hovelius reported an average loss of motion of 21 degrees of external rotation [28]. In our series, three patients had a minor or moderate loss of external rotation as reported by other authors; probably the tension of the subscapularis is increased by the rerouted muscles which pull it forward [5, 30].
Concerning secondary degenerative disease, we note one case in our series, and this is the first case reported following treatment with the Boytchev procedure. We think that it was not a consequence of the high number of dislocations (more than 200 dislocations in the patient concerned), because other authors like Chatterjee reported cases suffering very high numbers of dislocations (cases with 200, 250 and 500 dislocations) without degenerative disease, but rather that it was subsequent to stabilization by the force of the coracobrachialis and short head of the biceps muscles, acting as compressors of the head into the glenoid concavity and not only as a dynamic backstop [2]. The tip of the coracoid process with its muscles rerouted deep to the subscapularis also increases the compression from the subscapularis, which can hold the humeral head centred on the glenoid.
Shibata has also reported that the Boytchev procedure increases the pressure between the humeral head and the subscapularis tendon [18]. This pressure increases proprioceptive stimuli in the subscapularis tendon, and this accelerates the protective reflex needed to prevent shoulder dislocation. In our series, we did not observe any muscular weakness during the operative management (subscapularis, muscles attached to the coracoid process). In 2007, Lei-Sheng Jiang reported in his article that application of load to the conjoined tendon significantly reduced anterior displacement of the humeral head either with the capsule intact or with Bankart lesion simulated [31]. The most significant decrease of the anterior displacement occurred when the conjoined tendon was transferred beneath the subscapularis. Their findings show that the conjoined tendon per se has a stabilizing effect on unstable shoulders and therefore provide scientific support for the treatment of recurrent shoulder instability using the modified Boytchev procedure.
So we can assume, as other authors have done, for all types of open repair, that lesions, like bone deficiency, poor quality of soft tissues, decompensation of neuro-muscular control, hypoplasia, erosion or fracture of the glenoid rim, injuries of the rotator cuff, labrum, capsule (unhealed Bankart lesion), and ligaments are on the whole the main factors of shoulder instability and so lead to an unsteady glenohumeral stabilizing mechanism [24, 26 29]. Also like the majority of the authors who have reported on this technique, we thus confirm that the Boytchev procedure provides reliable stabilization of the shoulder and satisfactory function over time [2, 4, 5, 6, 12, 13, 14, 15, 16, 17, 18, 31, 32]. The fact remains that the gradation of results of the cited compiled studies confirms 441 satisfactory (excellent or good) results and 44 unsatisfactory (fair or poor), or 91% versus 9%, results which are obviously satisfactory, when generally compared with other procedures.
We can affirm that the Boytchev procedure is an effective technique and that other types of open repair do not offer better results in terms of stability, recovery of full range of motion, function and other complications. However, we do not plead for the superiority of this procedure and we insist on the fact that more studies are required to confirm these results.
Finally, we notice, as the majority of authors have done, that the Boytchev procedure provides reliable stabilization of the shoulder, satisfactory function over time and low recurrence rates (7.33% in 2% of the total dislocated shoulders reported on in the literature), and that it does not lead to more complications than other procedures. But even with these results, our conclusions must be drawn with caution, for a number of reasons: the limited amount of data available; the puzzlingly high recurrence rate in certain studies (Dalsgaard) [7]; the need for correct execution of the surgical procedure; the need for checks on the evolution of the patients; the importance of ensuring that the technique is in fact indicated; and the need for more cases to be studied, with longer-term follow up.
References
1 Allain J, Goutallier D, Glorion C: Long –term results of the Latarjet procedure for the treatment of anterior instability of the shoulder, JBoneJointSurg, 1998,80:841-52.
2 Anant Kumar Garg, Saankritya Ayan, Vikas K, Debi K, Kiran Kumar M, Biplab A: Modified Boytchev procedure for treatment of recurrent anterior dislocation of shoulder. Indian Journal of Orthopaedics. 2011 Jul-Aug; 45(4):336-340 DOI: 10.4103/0019-5413.82340
3 Bernal Gonzalez M, Cabrera Filtres N, Remon Davila, Xiomara de J. Alvarez Placeres L: Tratamiento quirurgico de la luxacion recidivante de hombro por la tecnica de Boytchev, Revista Cubana Ortop Traumatol, 2000, vol 14 :1-8
4 Boytchev B: Treatment of recurrent shoulder instability. Minerva Orthop 1951, 2:377-379
5 Chatterjee ND, Nath C, Pal AK, Baksi DP: Modified Boytchev procedure for the treatment of recurrent anterior dislocation of the shoulder. Int Orthop 2002, 26:7–9 DOI: 10.1007/s00264-001- 0303-7
6 Claes T: Boytchev anterior shoulder reconstruction: “no problem” surgery? Presented at the annual meeting of the American Orthopaedic Association, 1990, Boston,USA. (cited by Dalsgaard)
7 Conforty B: The results of the Boytchev procedure for treatment of recurrent dislocation of the shoulder. Int Orthop 1980, 4: 127- 132
8 Dalsgaard HL, Gothgen CB, Hoogmartens MJ: The Boytchev procedure for recurrent anterior dislocation of the shoulder: a controversial technique. Acta Orthop Belg 2000, 66:248–250
9 David Ip: Orthopedic-Traumatology:A resident’s guide. Second edition,Springer,2008: 252- 258 DOI 10.1007/978-3-540-75861-7
10 Deng J, Package J: Boytchev procedure for treatment of recurrent anterior dislocation of shoulder joint .Orthopaedic J China. 2003, 9:604-05
11 Ha’eri GB: Boytchev procedure for the treatment of anterior shoulder instability. Clin Orthop 1986, 206: 196-201
12 Han T, Zu Q, Xiang LB, Xian M: Modified Boytchev procedure for treatment of recurrent anterior dislocation of shoulder joint. J Clin Orthopaedics 2008, 6: 519-20
13 Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J: Primary anterior dislocation of the shoulder in young patients: A ten year prospective study, JBJS,1996, 78:1677- 84
14 Jader Riad Abumohor, Juan Montoya: Tratamiento de la inestabilidad anterior de hombro con la tecnica de Boytchev, Rev Med Hondur, 2009, 77 (1) 16-18 ,journal code :ISSN 0375-1112
15 Karlsson J, Magnusson L, Eperhed L, Hultenheim I, Lundin O, Kartus J: Comparison of open and arthroscopic stabilization for recurrent shoulder dislocation in patients with a Bankart lesion. Am J Sports Med, 2001, 29: 538-542
16 Lei-Sheng Jiang, Yi-Min Cui, Zhi-De Zhou, Li-Yang Dai: Stabilizing effect of the transferred conjoined tendon on shoulder stability, Knee surgery, Sports Traumatology, Arthroscopy, 2007, 15,6: 800-805. DOI:10.1007/s00167-006-0239-y
17 Mendez Caballos J.A, Saenz Lopez de Rueda F, Zamora Navas P, Flores Gallego F.J, Luna Sanchez C, Huerta Valderas J: Tratamiento quirurgico de la luxacion recidivante de hombro por transposicion del coraco biceps, Rev Esp de Cir Ost,1985, 20, 39-45.
18 Morrey BF, Janes JM: Recurrent anterior dislocation of the shoulder: long term follow up of the Putti Platt and Bankart procedures. J Bone Joint Surg.1976, 58 A: 252-256
19 O’Driscoll SW, Evans DC: The DuToit staple capsulorrhaphy for recurrent anterior dislocation of the shoulder: Twenty years of experience in six Toronto hospitals. American shoulder and Elbow Surgeons 4th Open Meeting, Atlanta, 1988.
20 Ping L, Chen F: Improved Boytchev treatment of habitual anterior dislocation of 15 cases. J Integr Tradit West Med China. 2007, 2: 513-14
21 Roca LA, Ramos-Vertiz: Luxacion erecta de hombro. Rev San Mil Arg.1962, 61: 135.
22 Rockwood C.A Jr, Green D.P: Part 2: Dislocations about the shoulder. J.B1.1, 2nd Ed, eds. Lippincot,Vo, Philadelphia,1984
23 Rowe CR, Patel D, Southmayd WW: The Bankart procedure: A long-term end-result study, JBJS 60-A,1978,1-16.
24 Rowe CR, Zarins B, Ciullo JV: Recurrent anterior dislocation of the shoulder after surgical repair: Apparent causes of failure and treatment. J Bone Joint Surg 66A:159, 1984.
25 Rowe CR: Prognosis in dislocations of the shoulder, J Bone Joint Surg., 1956, 38:957-977
26 Samilson RL, Prieto V: Dislocation arthropathy of the shoulder. J Bone and Joint Surg., 1983, 65- A: 456-460.
27 Shibata Y, Midorikawa K, Ogata K, Izaki T: Modified Boytchev and its combined operation for traumatic unstable shoulder. Shoulder Joint. 1999, 23: 327-1
28 Shibata Y, Honjo N, Shinoda T, Kumano T, Naito M (2004) Pressure between the humeral head and the subscapularis tendon after the modified Boytchev procedure. J Shoulder Elbow Surg 13: 170–173, DOI:10.1016/j.jse.2003.12.010
29 Ungersbock A, Michel M, Hertel R: Factors influencing the results of a modified Bankart procedure. J Shoulder Elbow Surg 4: 365-369, 1995.
30 Warren-Smith CD, Wallace WA, Ebrahimzade AR, Pailthorpe CA: Pitfalls with the Boytchev operation for recurrent anterior shoulder dislocation. Presented at the fourth International Conference on surgery of the shoulder, October 4-7, 1999, New York, USA. (cited by Dalsgaard)
31 Zabinski SJ, Callaway GH, Cohen S, Warren RF: Long Term Results of Revision Shoulder Stabilization. American Shoulder and Elbow Surgeons Meeting, La Quinta, CA, 1995. .
32 Zamora-Navas P, Borras Verdera A, Porras Garcia J, Padilla Marquez A, Linares P: Long-term results of the Boytchev procedure for the treatment of recurrent dislocation of the shoulder. Acta Orthopaedica Belgica, 2001, 67-3: 233-235
| How to Cite this article: Benabdallah O, Khamlichi A, Recurrent Anterior Shoulder Dislocation: Boytchev Treatment. Trauma International May-Aug 2016; 2(2): 31-39. |